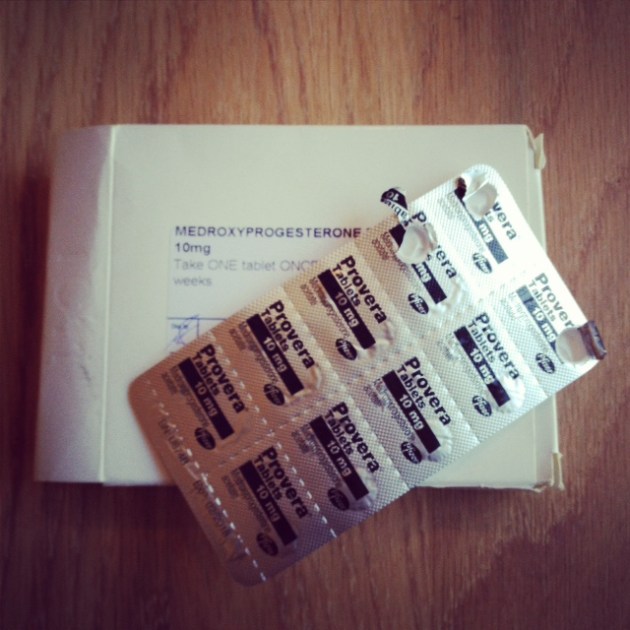
Today is a milestone day. Ok, so it’s not exactly on a par with diagnosis day or pathology results day (just a few of the compulsory days Breast Cancer likes to throw in to keep us entertained). But, that doesn’t make it any less meaningful. No, today is the day I come off Provera (my progesterone hormone). That means, in a few days time (if my body plays ball), the fertility side of my treatment will begin. Self injecting here I come!
Moments in time don’t have to be monumental to make it as milestones. When you are strapped into a body corset, even getting to the end of the road can feel like a huge achievement! So here is a glimpse into my world of the major – and not so major milestones – that have made a mark in my diary these last few months. I hope this will help those facing the cancer challenge in the future to understand a bit more about timeframes and what to expect.
1) 24 December: Lump discovery day
Arguably the most important day (and most valuable shower) of my life. I took the discovery seriously, but am glad to report, it didn’t put me off the Christmas ham.
2) 25 December: Proposal day
Ok, so not fundamental to the story, but it’s a lot easier talking about losing a boob and making embryos when you have a man by your side (and a ring on your finger). I am a lucky lady.
3) 27 December: GP referral day
Not the most reassuring of visits I’ll admit, but the doctor acted really fast and referred me straight away. I know a lot of young women are told to come back at another point in their cycle to see whether the lump has changed size, but thankfully, due to it being Christmas, I got my referral. Just another reason to love Christmas!
4) 9 January: Hospital appointment day
Was planned in as the morning before, but due to work commitments, I moved it to the Thursday morning. I know how stupid that sounds, but I really didn’t believe it was anything other than a breast mouse. Let’s just say, I have learned my lesson (and missed a fabulous annual client lunch that day as punishment). What started as a quick ‘feel’ turned into an ultrasound, a few biopsies and a rather awkward conversation with two consultants (they didn’t say cancer, but they did ask about my family history A LOT).
5) 17 January: Diagnosis day
Not a day I’ll forget…ever! Crying, mammogram, more crying, truck load of leaflets and, you guessed it, more crying.
6) 18 January: The day that taught me the value of friendship
Afternoon tea at the Modern Pantry was made all the more sweet with a close friend at my side. Having hidden away for months, this day encouraged me to get out my phone and start planning (trips to Sketch, nights with Darius, relaxing walks and home visits). I love my friends and the colour they bring to my days.
7) 23 January: MRI day
Four needles, one arm full of contrast dye and a noisy test to determine whether or not I could have a lumpectomy.
8) 25 January: Feeling human day
I had a facial. No one mentioned cancer. I walked into a shop (ok, so I was buying track suit bottoms and zip up tops) and someone told me I looked and smelled great. I smiled. It felt good.
9) 27 January: Diagnosis day (part two)
More cancer, another biopsy, a trip on a secret staff bus, a plastic surgeon meeting, pre-op testing and a lot of tummy squeezing. The mastectomy is on, the tummy is borderline.
10) 31 January: Fat testing day
One CT scan and one feel-like-you-are-wetting-yourself moment to check whether I had a good blood vessel in my tummy to transfer to my boobie.
11) 1 February: The day I decided to start this blog
A major mental milestone, this blog helps me stay positive, while keeping my loved ones informed and helping others diagnosed with the big C!
12) 4 February: Carbo-loading day
Ok, so with the volume of chocolate coming through the letterbox on a daily basis, this was more like a two-week period. But, on this day, at a work away session, I ate a lot. I believe this was a major step forward for tummy and will always think about it when rubbing aqueous cream into new boobie.
13) 10 February: Decision day
Tummy confirmed as new boobie. Did a little dance (away from the surgeons of course)!
14) 14 February: Provera day one
The countdown to freezing embryos begins. Won’t mention what happened to Duncan that day. More of a fertility milestone for him than me. And on Valentine’s Day!
15) 15 February: Last supper with D day
Sounds a bit dramatic, but it was actually a beautiful meal at the Cutty Sark pub that reminded me of the importance of taking time out to savour special moments with loved ones.
16) 19 February: Pre-assessment and mobile off day
Memorable not because I found out about leeches, physio moves and arm measuring, but because I turned my work emails off on my Blackberry for the first time in a long time. The red button now only flashes to alert me of good wishes.
17) 20 February: the day I tried my first ever Nandos
Ok, don’t judge me. Not quite the last supper I had imagined. Couldn’t resist. First time ever – and with my parents.
18) 21 February: Surgery day
Wasn’t around much, but hear it went well. Got a new boobie. Got rid of cancer. Not a bad day.
19) 22 February: The day I survived
Owwwwwwwwwww! It hurt, but I got through it, and that is all that matters.
20) 23 February: The day I got up
Getting out of bed is only a big event if you thought you’d never get out again the day before.
21) 24 February: The day the drains started coming out
They don’t hurt if you breathe in and out three times and follow the nurse’s instructions. Go to your happy place and you’ll be fine.
22) 25 February: Big reveal day
I don’t think I’ll ever forget the mirrors or the tears. I did manage to wash myself and pull my big knickers up though, so it wasn’t all bad. I also got rid of that moving mattress (certainly something worth celebrating).
23) 26 February: The day I got released
Hospital day 5 means home time. Felt good sinking down into our old mattress and getting settled with my home comforts.
24) 1 March: The day I did nothing
Having overworked my arm the day before, today was a day of reading and film watching. Never underestimate the restorative power of nothing. I have been too busy in life to notice.
25) 3 March: The day I finished my first post-surgery book
I love books, but could never get into them after my hip surgery. I take this as a good sign my brain is starting to fire again.
26) 5 March: The day I dressed myself
Wouldn’t have made this a milestone a few weeks ago. It’s amazing how much excitement can be gained from putting your socks on. I also passed wound care today, so one step forward.
27) 6 March: The day I walked in the park
Ok, so we had to drive there, but Greenwich Park had never looked so inviting with the early signs of spring. I even got to see the deer and admire the view.
28) 7 March: Pathology results day
The first day of the rest of my life. A big meeting that reinforced the importance of seeking out milestones and making a difference every day. Friday was also the day my wonderful nurse of a mum went back home to leave Duncan and I to fend for ourselves. I am happy to report that we are doing pretty well. Duncan is spending most of his time trying to stop me lifting things (I have resorted to painting my nails in the hope that the frustration of chipping the paint will stop me in my tracks) and we did have a rather interesting discussion about the merits of a scrubbing brush when doing the washing up (he is going to buy one this weekend).
29) 8 March: Duncan does the washing up day (and gets a quick look)
A monumental life event. Ok, so he struggled with the pan, but he did great (even without a scrubbing brush). His reaction to the ‘new’ me was thoughtful and kind. He even towel-dried my back when I couldn’t reach. I also got to remove the sticky mesh on my tummy and the final steri-strips on my boob, so am starting to look less like an accident victim.
30) 9 March: Bye bye Provera day
The window to help preserve my fertility is starting to open. Have also just had a lovely lunch outside for the first time this year.
They may not be big, but for me, each one of these milestones has made 2014 one of the busiest and most emotional yet – and it’s still only March. Each date has made such a lasting impression, I didn’t even need to consult a diary to write this post.
There will be many more cancer milestones (and more tenuous ones) to come (from chemo day one to radiotherapy planning day and the day I get my first tattoo) and I intend to embrace and smile in the face of each one. After all, a life without milestones, however small, is not really a life at all.
So, raise a glass to milestones. May you all have many happy ones this year.